Chloroquine - Wikipedia
As this is being proposed as a cure for Covid, it's important to know the adverse effects, drug interactions, etc. Personally, I'd rather not have to take it, especially because of the possible toxic effects on the retinas, and cardiomyopathy (a generalized disease state of the heart muscle). However, it certainly is not the worst big pharma has to throw at us. As chloroquine is most often given with other drugs, the statistics, as to serious side effects and toxicity, may be skewed. Despite the name, and it's anti-malarial activity and purpose, it is only mildly similar to the quinine molecule. Chloroquine inhibits Thiamine (Vitamin B1) uptake, so better take extra Thiamine if you take chloroquine. 11 Signs and Symptoms of Thiamine (Vitamin B1) Deficiency - (serious health problems). Hope this info helps.
Chloroquine is a medication used to prevent and to treat malaria in areas where malaria is known to be sensitive to its effects.[1] Certain types of malaria, resistant strains, and complicated cases typically require different or additional medication.[1] Occasionally it is used for amebiasis that is occurring outside the intestines, rheumatoid arthritis, and lupus erythematosus.[1] It is taken by mouth.[1] It is also being used experimentally to treat COVID-19 as of 2020.[2] It was found to be an inhibitor of SARS coronavirus in 2004 and 2005.[3][4]
Common side effects include muscle problems, loss of appetite, diarrhea, and skin rash.[1] Serious side effects include problems with vision, muscle damage, seizures, and low blood cell levels.[1] It appears to be safe for use during pregnancy.[1][5] Chloroquine is a member of the drug class 4-aminoquinoline.[1] It works against the asexual form of malaria inside the red blood cell.[1]
Chloroquine was discovered in 1934 by Hans Andersag.[6][7] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[8] It is available as a generic medication.[1] The wholesale cost in the developing world is about US$0.04.[9] In the United States, it costs about US$5.30 per dose.[1]
Medical uses
Malaria
Chloroquine has long been used in the treatment or prevention of malaria from Plasmodium vivax, P. ovale, and P. malariae, excluding the malaria parasite Plasmodium falciparum, for it started to develop widespread resistance to it.[10][11]
Chloroquine has been extensively used in mass drug administrations, which may have contributed to the emergence and spread of resistance. It is recommended to check if chloroquine is still effective in the region prior to using it.[12] In areas where resistance is present, other antimalarials, such as mefloquine or atovaquone, may be used instead. The Centers for Disease Control and Prevention recommend against treatment of malaria with chloroquine alone due to more effective combinations.[13]
Amebiasis
In treatment of amoebic liver abscess, chloroquine may be used instead of or in addition to other medications in the event of failure of improvement with metronidazole or another nitroimidazole within 5 days or intolerance to metronidazole or a nitroimidazole.[14]
Rheumatic disease
As it mildly suppresses the immune system, it is used in some autoimmune disorders, such as rheumatoid arthritis and lupus erythematosus.[1]
Side effects
Side effects include neuromuscular, hearing, gastrointestinal, brain, skin, eye, cardiovascular (rare), and blood reactions.[15]
- Seizures[15]
- Deafness or tinnitus.[15]
- Nausea, vomiting, diarrhea, abdominal cramps, and anorexia.[15]
- Mild and transient headache.[15]
- Skin itchiness, skin color changes, hair loss, and skin rashes.[15]
- Chloroquine-induced itching is very common among black Africans (70%), but much less common in other races. It increases with age, and is so severe as to stop compliance with drug therapy. It is increased during malaria fever; its severity is correlated to the malaria parasite load in blood. Some evidence indicates it has a genetic basis and is related to chloroquine action with opiate receptors centrally or peripherally.[16]
- Unpleasant metallic taste
- This could be avoided by "taste-masked and controlled release" formulations such as multiple emulsions.[17]
- Chloroquine retinopathy
- May be irreversible.[15] This occurs with long-term use over many years or with high doses. Patients on long-term chloroquine therapy should be screened at baseline and then annually after five years of use.[18] Patients should be screened for vision changes such as blurring of vision, difficulty focusing, or seeing half an object.[15]
- Hypotension and electrocardiographic changes[15][19]
- This manifests itself as either conduction disturbances (bundle-branch block, atrioventricular block) or cardiomyopathy – often with hypertrophy, restrictive physiology, and congestive heart failure. The changes may be irreversible. Only two cases have been reported requiring heart transplantation, suggesting this particular risk is very low. Electron microscopy of cardiac biopsies show pathognomonic cytoplasmic inclusion bodies.
- Pancytopenia, aplastic anemia, reversible agranulocytosis, low blood platelets, neutropenia.[20]
Pregnancy
Chloroquine has not been shown to have any harmful effects on the fetus when used for malarial prophylaxis.[21] Small amounts of chloroquine are excreted in the breast milk of lactating women. However, because this drug can be safely prescribed to infants, the effects are not harmful. Studies with mice show that radioactively tagged chloroquine passed through the placenta rapidly and accumulated in the fetal eyes which remained present five months after the drug was cleared from the rest of the body.[20][22] It is still advised to prevent women who are pregnant or planning on getting pregnant from traveling to malaria-risk regions.[21]
Elderly
There is not enough evidence to determine whether chloroquine is safe to be given to people aged 65 and older. However, the drug is cleared by the kidneys and toxicity should be monitored carefully in people with poor kidney functions.[20]
Drug interactions
- Ampicillin- levels may be reduced by chloroquine
- Antacids- may reduce absorption of chloroquine
- Cimetidine- may inhibit metabolism of chloroquine; increasing levels of chloroquine in the body
- Cyclosporine- levels may be increased by chloroquine
- Kaolin- may reduce absorption of chloroquine
- Mefloquine- may increase risk of convulsions[20]
Overdose
Chloroquine is very dangerous in overdose. It is rapidly absorbed from the gut. In 1961, published studies showed three children who took overdoses died within 2.5 hours of taking the drug. While the amount of the overdose was not cited, the therapeutic index for chloroquine is known to be small.[23] Symptoms of overdose include headache, drowsiness, visual disturbances, nausea and vomiting, cardiovascular collapse, seizures, and sudden respiratory and cardiac arrest.[20]
An analog of chloroquine – hydroxychloroquine – has a long half-life (32–56 days) in blood and a large volume of distribution (580–815 L/kg).[24] The therapeutic, toxic and lethal ranges are usually considered to be 0.03 to 15 mg/l, 3.0 to 26 mg/l and 20 to 104 mg/l, respectively. However, nontoxic cases have been reported up to 39 mg/l, suggesting individual tolerance to this agent may be more variable than previously recognised.[24]
Pharmacology
- Absorption: Rapid and almost completely
- Distribution: Widely distributed into body tissues
- Protein binding: 55%
- Metabolism: Partially hepatic to main metabolite, desethylchloroquine
- Excretion: Urine (≥50% as unchanged drug); acidification of urine increases elimination
Chloroquine has a very high volume of distribution, as it diffuses into the body's adipose tissue. Chloroquine and related quinines have been associated with cases of retinal toxicity, particularly when provided at higher doses for longer times. Accumulation of the drug may result in deposits that can lead to blurred vision and blindness. With long-term doses, routine visits to an ophthalmologist are recommended.[citation needed]
Chloroquine is also a lysosomotropic agent, meaning it accumulates preferentially in the lysosomes of cells in the body. The pKa for the quinoline nitrogen of chloroquine is 8.5, meaning it is about 10% deprotonated at physiological pH as calculated by the Henderson-Hasselbalch equation. This decreases to about 0.2% at a lysosomal pH of 4.6. Because the deprotonated form is more membrane-permeable than the protonated form, a quantitative "trapping" of the compound in lysosomes results. (A quantitative treatment of this phenomenon involves the pKas of all nitrogens in the molecule; this treatment, however, suffices to show the principle.)[citation needed]
The lysosomotropic character of chloroquine is believed to account for much of its antimalarial activity; the drug concentrates in the acidic food vacuole of the parasite and interferes with essential processes. Its lysosomotropic properties further allow for its use for in vitro experiments pertaining to intracellular lipid related diseases,[25][26] autophagy, and apoptosis.[27]
Mechanism of action
Malaria
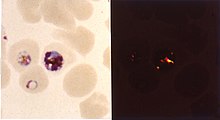
Inside red blood cells, the malarial parasite, which is then in its asexual lifecycle stage, must degrade hemoglobin to acquire essential amino acids, which the parasite requires to construct its own protein and for energy metabolism. Digestion is carried out in a vacuole of the parasitic cell.[citation needed]
Hemoglobin is composed of a protein unit (digested by the parasite) and a heme unit (not used by the parasite). During this process, the parasite releases the toxic and soluble molecule heme. The heme moiety consists of a porphyrin ring called Fe(II)-protoporphyrin IX (FP). To avoid destruction by this molecule, the parasite biocrystallizes heme to form hemozoin, a nontoxic molecule. Hemozoin collects in the digestive vacuole as insoluble crystals.[citation needed]
Chloroquine enters the red blood cell by simple diffusion, inhibiting the parasite cell and digestive vacuole. Chloroquine then becomes protonated (to CQ2+), as the digestive vacuole is known to be acidic (pH 4.7); chloroquine then cannot leave by diffusion. Chloroquine caps hemozoin molecules to prevent further biocrystallization of heme, thus leading to heme buildup. Chloroquine binds to heme (or FP) to form the FP-chloroquine complex; this complex is highly toxic to the cell and disrupts membrane function. Action of the toxic FP-chloroquine and FP results in cell lysis and ultimately parasite cell autodigestion. In essence, the parasite cell drowns in its own metabolic products.[28] Parasites that do not form hemozoin are therefore resistant to chloroquine.[29]
Resistance in malaria
Since the first documentation of P. falciparum chloroquine resistance in the 1950s, resistant strains have appeared throughout East and West Africa, Southeast Asia, and South America. The effectiveness of chloroquine against P. falciparum has declined as resistant strains of the parasite evolved. They effectively neutralize the drug via a mechanism that drains chloroquine away from the digestive vacuole. Chloroquine-resistant cells efflux chloroquine at 40 times the rate of chloroquine-sensitive cells; the related mutations trace back to transmembrane proteins of the digestive vacuole, including sets of critical mutations in the P. falciparum chloroquine resistance transporter (PfCRT) gene. The mutated protein, but not the wild-type transporter, transports chloroquine when expressed in Xenopus oocytes (frog's eggs) and is thought to mediate chloroquine leak from its site of action in the digestive vacuole.[30] Resistant parasites also frequently have mutated products of the ABC transporter P. falciparum multidrug resistance (PfMDR1) gene, although these mutations are thought to be of secondary importance compared to Pfcrt. Verapamil, a Ca2+ channel blocker, has been found to restore both the chloroquine concentration ability and sensitivity to this drug. Recently, an altered chloroquine-transporter protein CG2 of the parasite has been related to chloroquine resistance, but other mechanisms of resistance also appear to be involved.[31] Research on the mechanism of chloroquine and how the parasite has acquired chloroquine resistance is still ongoing, as other mechanisms of resistance are likely.[citation needed]
Other agents which have been shown to reverse chloroquine resistance in malaria are chlorpheniramine, gefitinib, imatinib, tariquidar and zosuquidar.[32]
Antiviral
Chloroquine has antiviral effects,[33] which work by increasing endosomal pH resulting in impaired virus/cell fusion that requires a low pH.[34][35]
Chloroquine also seems to act as a zinc ionophore, thereby allowing extra cellular zinc to enter inside the cell and inhibit viral RNA dependant RNA polymerase.[36][37]
Other
Chloroquine inhibits thiamine uptake.[38] It acts specifically on the transporter SLC19A3.
Against rheumatoid arthritis, it operates by inhibiting lymphocyte proliferation, phospholipase A2, antigen presentation in dendritic cells, release of enzymes from lysosomes, release of reactive oxygen species from macrophages, and production of IL-1.
History
In Peru the indigenous people extracted the bark of the Cinchona plant[39] trees and used the extract (Chinchona officinalis) to fight chills and fever in the seventeenth century. In 1633 this herbal medicine was introduced in Europe, where it was given the same use and also began to be used against malaria.[40] The quinoline antimalarial drug quinine was isolated from the extract in 1820, and chloroquine is an analogue of this.
Chloroquine was discovered in 1934 by Hans Andersag and coworkers at the Bayer laboratories, who named it "Resochin".[41] It was ignored for a decade because it was considered too toxic for human use. During World War II, United States government-sponsored clinical trials for antimalarial drug development showed unequivocally that chloroquine has a significant therapeutic value as an antimalarial drug. It was introduced into clinical practice in 1947 for the prophylactic treatment of malaria.[42]
Names
Brand names include Chloroquine FNA, Resochin, Dawaquin, and Lariago.[43]
Research
COVID-19
In late January 2020 during the 2019–20 coronavirus outbreak, Chinese medical researchers stated that exploratory research into chloroquine and two other medications, remdesivir and lopinavir/ritonavir, seemed to have "fairly good inhibitory effects" on the SARS-CoV-2 virus, which is the virus that causes COVID-19. Requests to start clinical testing were submitted.[44][45] Chloroquine had been also proposed as a treatment for SARS, with in vitro tests inhibiting the SARS-CoV virus.[46]
On 19 February 2020, preliminary results found that chloroquine may be effective and safe in treating COVID-19 associated pneumonia.[47] There is evidence to indicate the efficacy of chloroquine phosphate against SARS-CoV-2 in vitro on Vero cells.[44] The Guangdong Provincial Department of Science and Technology and the Guangdong Provincial Health and Health Commission issued a report stating that chloroquine phosphate "improves the success rate of treatment and shortens the length of patient’s hospital stay" and recommended it for people diagnosed with mild, moderate and severe cases of novel coronavirus pneumonia.[48]
Chloroquine has been recommended by Chinese, South Korean and Italian health authorities for the treatment of COVID-19,[49][50][unreliable medical source?] although these agencies noted contraindications for people with heart disease or diabetes.[51] In February 2020, both drugs were shown to effectively inhibit COVID-19 in vitro,[44] but a further study concluded that hydroxychloroquine was more potent than chloroquine, with a more tolerable safety profile.[52] Preliminary results from a trial suggested that chloroquine is effective and safe in COVID-19 pneumonia, "improving lung imaging findings, promoting a virus-negative conversion, and shortening the disease course."[47]
Other viruses
Chloroquine is being considered in pre-clinical models as a potential agent against chikungunya fever.[53]
Other
The radiosensitizing and chemosensitizing properties of chloroquine are beginning to be exploited in anticancer strategies in humans.[54][55] In biomedicinal science, chloroquine is used for in vitro experiments to inhibit lysosomal degradation of protein products.
References (more at link.)
Comment
-
Comment by James Roberts on March 20, 2020 at 9:00pm
-
Other than what I outlined in the opening paragraph, the most significant negative quality of chloroquine is that it suppresses the immune system somewhat. It is something to think about when choosing whether or not to take chloroquine.
"Destroying the New World Order"
THANK YOU FOR SUPPORTING THE SITE!
Latest Activity
- Top News
- ·
- Everything
The Proper Definition Rather Than Democrat Rhetoric
Peter Sellers - The Party (opening scene)
Disgraced Former CNN Anchor Don Lemon Arrested
Our Crazy Modern World
2DF36465-A826-443C-A3A8-6638BC1D4FFA
G_LrzqtXMAAhT7w
© 2026 Created by truth.
Powered by
![]()


You need to be a member of 12160 Social Network to add comments!
Join 12160 Social Network